Toxoplasmosis is a systemic, zoonotic infection caused by Toxoplasma gondii, a protozoan parasite that affects mammals and birds. Although many people are unaware of it, toxoplasmosis is of particular concern for pregnant individuals, due to its potential risks to the fetus. It is estimated that one-third of the world’s population is infected with this parasite.Cats and other members of the Felidae family serve as both intermediate and, uniquely, the definitive hosts for T. gondii. Intermediate hosts include a wide variety of mammals and birds, including humans.
What is Toxoplasma gondii?
Toxoplasma gondii is a typical coccidian parasite belonging to the family Sarcocystidae and the genus Toxoplasma, within the protozoan group.
Transmission
The forms of Toxoplasma gondii responsible for transmission are primarily oocysts and tissue cysts.
The organism develops within the intestinal cells of cats. Cats typically become infected by consuming raw meat or rodents. Once inside the intestinal cells, the parasite enters in its tachyzoite (trapezoid) form using its cone-shaped apical structure, and begins to multiply.
Where Can Toxoplasma gondii Be Found?
- Cat feces
- Soil or cat litter contaminated with infected feces
- Undercooked or raw meat
- Cured, raw meat products such as Parma ham or salami
- Unpasteurized milk and eggs
Although Toxoplasma gondii cannot be transmitted from human to human via direct contact, it can be passed from an infected mother to her unborn child.
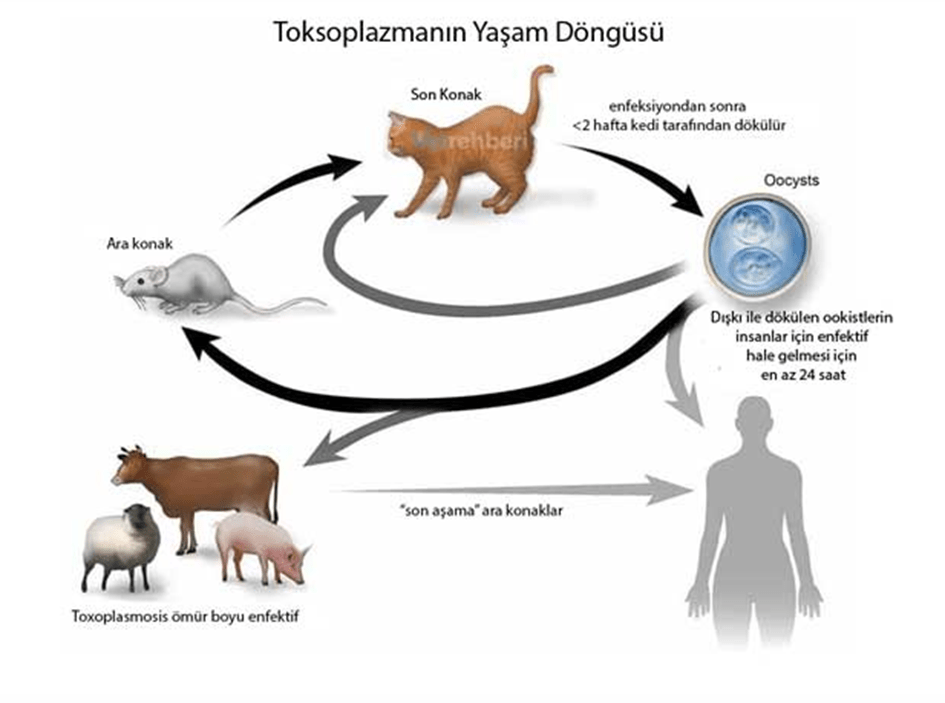
Photo by https://vetrehberi.com/toxoplasma/
Clinical Findings in Cats
It has been reported that cats infected with Toxoplasma gondii generally do not exhibit noticeable clinical signs, although minor issues related to the enteroepithelial (intestinal) cycle may occasionally occur. Experimental studies have shown that 10–20% of cats orally infected with tissue cysts may develop diarrhea lasting 1–2 weeks, attributed to the replication of the parasite within the intestinal epithelium.
Following primary infection, extensive intracellular replication of tachyzoites can lead to fatal extraintestinal toxoplasmosis, with the infection potentially spreading to the liver, lungs, brain, and pancreatic tissues.
It has also been noted that congenital transmission from an infected mother to her kittens can result in extraintestinal toxoplasmosis, which frequently affects the lungs or liver and may lead to death.
In cats with compromised immune systems, disseminated toxoplasmosis has been observed. Clinical signs in such cases may include depression, loss of appetite, fever, abdominal fluid accumulation (ascites), jaundice, and dyspnea (difficulty breathing).
In chronic toxoplasmosis, affected cats may exhibit:
- Uveitis
- Cutaneous lesions
- Persistent fever
- Muscle hypersensitivity
- Myocarditis with arrhythmia
- Weight loss
- Anorexia
- Paralysis
- Ataxia
- Jaundice
- Diarrhea
- Respiratory distress
Relationship with Pregnancy
As mentioned in the section on transmission, toxoplasmosis cannot be transmitted through direct person-to-person contact, but it can be passed from an infected pregnant woman to her unborn child. This vertical transmission is only possible if the woman acquires the infection during pregnancy.
One of the most important preventive measures is to ensure that cat feces are cleaned within 24 hours by someone other than the pregnant woman, as oocysts require time to become infective.
- If a baby is born infected due to the mother contracting the parasite during pregnancy or up to three months prior to conception, the condition is referred to as congenital toxoplasmosis.
Congenital Toxoplasmosis
When tachyzoite forms of Toxoplasma gondii are acquired during pregnancy, they may cross the placenta and infect the fetus. Due to the immaturity of the fetal immune system, this condition is particularly feared by clinicians.
Congenital toxoplasmosis may lead to the following clinical outcomes:
- Cerebral calcifications
- Chorioretinitis, which may manifest later in life
- Macrocephaly due to hydrocephalus
- Microcephaly
- Seizures
- Skin rashes and jaundice
Antibody Testing in Pregnant Women
It is recommended to evaluate the IgG antibody levels either 3–4 months before conception or as soon as pregnancy is detected.
If protective antibody levels (IgG) are present, there is no risk of infection to the baby.
If antibody levels are low or absent, regular serological monitoring throughout pregnancy is essential to ensure early detection and intervention.
This blog post has been verified by veterinarian YUNUS EMRE AŞICI
Resources:
Dubey JP, (2010). Toxoplasmosis of Animals and Man. Second Edition, CRC Pres, New York.
Milli ÜH, Hazıroğlu R, (2000). Veteriner Patoloji. Medipress, Malatya
Murray, Patrick R. (2013). Medical microbiology. 7th edition. Rosenthal, Ken S., Pfaller, Michael A. Philadelphia: Elsevier/Saunders. ISBN 978-0-323-08692-9. OCLC 778040143.
Pekmezci, D., & Pekmezci, G. Z. (2016). Toksoplazmozis Kedilerde Davranışsal Değişikliklere Neden Olabilir mi?. Etlik Veteriner Mikrobiyoloji Dergisi, 27(2), 149-154.
ÖNCEL, T. toncel@penvet. gov. tr.
Beder, D., & Taşbent, F. E. (2020). Genel Özellikleri ve Laboratuvar Tanısı ile Toxoplasma gondii Enfeksiyonları. Türkiye Parazitolojii Dergisi, 44(2), 94.
McConnell JF, Sparkes AH, Blunden AS, Neath PJ, Sansom J, (2007). Eosinophilic fibrosing gastritis and toxoplasmosis in a cat. JFMS. 9(1), 82-88.
Lappin MR, (2010). Update on the diagnosis and management of Toxoplasma gondii infection in cats. Topics in Compan An Med. 25(3), 136-141.
Beatty J, Barrs, V, (2003). Acute toxoplasmosis in two cats on cyclosporine therapy. Aust Vet J. 81, 339.